Sometimes called "wear-and-tear" arthritis, and also called degenerative joint disease, osteoarthritis is a common condition that many people develop during middle age or older. Although osteoarthritis can affect any joint in the body, it most often develops in weight-bearing joints, such as the hip and knee.
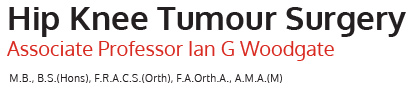
In osteoarthritis, the cartilage in the hip joint becomes damaged and gradually wears away over time. As the cartilage wears away, it becomes frayed and rough, and the protective joint space between the bones decreases. This can result in bone rubbing on bone. To make up for the lost cartilage, the damaged bones may start to grow outward and form bone spurs (osteophytes).
orthoinfo.aaos.org
Cause
Osteoarthritis has no single specific cause, but there are certain factors that may make you more likely to develop the disease, including:
- Increasing age
- Family history of osteoarthritis
- Previous injury or trauma to the hip joint
- Previous avascular necrosis (osteonecrosis)
- Obesity
- Improper formation of the hip joint at birth, a condition known as developmental dysplasia of the hip
- Childhood/adolescent hip conditions, such as Perthes disease or slipped capital femoral epiphysis
Even if you do not have any of the risk factors listed above, you can still develop osteoarthritis.
Symptoms
The most common symptom of hip osteoarthritis is pain around the hip joint. Usually, the pain develops slowly and worsens over time, although sudden onset is also possible. Pain and stiffness may be worse in the morning, or after sitting or resting for a while. Over time, painful symptoms may occur more frequently, including during rest or at night. Additional symptoms may include:
- Pain in your groin or thigh that radiates to your buttocks or your knee
- Pain that flares up with vigorous activity
- Stiffness in the hip joint that makes it difficult to walk or bend
- "Locking" or "catching" of the joint
- A grinding noise (crepitus) during movement caused by loose fragments of cartilage and other tissue interfering with the smooth motion of the hip
- Decreased range of motion in the hip that affects the ability to walk, put on shoes and socks, wipe your feet, or cut your toenails
- Difficulty with transfers in and out of chairs or cars
- A limp may develop
- Leg length discrepancy
- Increased joint pain with rainy weather.
Diagnosis
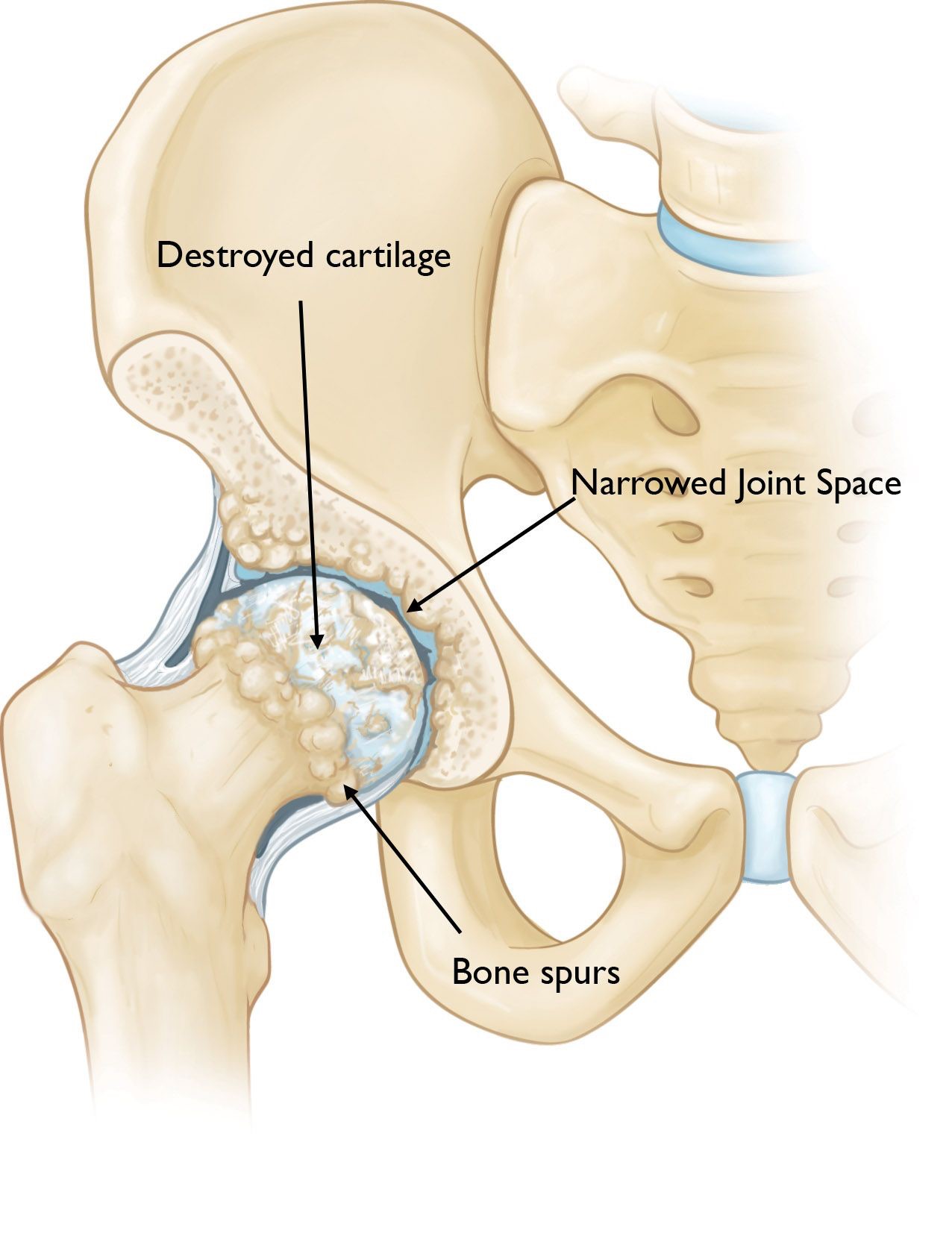
History and physical examination is initially performed, including an assessment of functional impairment. This will determine which further diagnostic tests will be needed for confirmation of diagnosis, including Xrays. MRI or other scans are sometimes required. Blood tests may be needed to exclude other conditions that may cause similar symptoms, or if you have co-morbid conditions that may impact on subsequent treatment options.
orthoinfo.aaos.org
(Left) In this x-ray of a normal hip, the space between the ball and socket indicates healthy cartilage. (Right) This x-ray of an arthritic hip shows severe loss of joint space and bone spurs.
Treatment of Osteoarthritis of the Hip
Although there is no cure for osteoarthritis, there are many treatment options to help you manage pain and stay active.
Nonsurgical Treatment
As with other arthritic conditions, the early treatment of hip osteoarthritis is nonsurgical, and can include:
- Lifestyle modifications. - Some changes in your daily life can protect your hip joint and slow the progress of osteoarthritis.
- Minimizing activities that aggravate the condition, such as climbing stairs.
- Switching from high-impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling) will put less stress on your hip.
- Losing weight can reduce stress on the hip joint, resulting in less pain and increased function.
- Physical therapy - Specific exercises can help increase range of motion and flexibility, as well as strengthen the muscles in your hip and leg, and this exercise programme will need to be individualized to meet your needs and lifestyle.
- Assistive devices - Using walking supports like a cane, crutches, or a walker can improve mobility and independence. Using assistive aids like a long-handled reacher to pick up low-lying things will help you avoid movements that may cause pain. Even long shoehorns are available to aid with putting on shoes.
- Medications - If your pain affects your daily routine, or is not relieved by other nonsurgical methods, medication may be advised as part of your treatment plan:
- Paracetamol is an over-the-counter pain reliever that can be effective in reducing mild arthritis pain. Like all medications, however, over-the-counter pain relievers can cause side effects and interact with other medications you are taking. Be sure to discuss potential side effects with A/Prof Woodgate.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) may relieve pain and reduce inflammation.
- Opioids are occasionally used short-term prior to and after surgical intervention.
- Steroids are powerful anti-inflammatory agents that can be injected into the painful joint to give temporary relief.
Surgical Treatment
Surgical treatment is indicated for failure of the conservative management programme, or when the hip pain is so severe that it affects your ability to carry out normal activities.
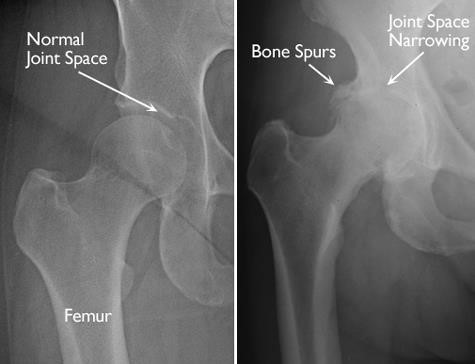
The most common surgical procedure recommended is total hip replacement. Total hip replacement is a surgical procedure in which the damaged cartilage and bone is removed from the hip joint and replaced with artificial components. It is quoted as one of the most successful operations with regard to outcomes, and with high patient satisfaction (averaging over 95%).
Although complications are possible with any surgery, A/Prof Woodgate will take steps to minimize the risks. The most common complications of the surgery include:
- Infection
- Excessive bleeding
- Blood clots (deep venous thrombosis – DVT)
- Hip dislocation / instability
- Limb length inequality
- Damage to blood vessels or nerves
- Hip component failure or loosening
- Heterotopic ossification (abnormal formation of extra bone around the capsule and in the muscles around the hip joint which will limit motion).
orthoinfo.aaos.org
Recovery
After any type of surgery for osteoarthritis of the hip, there is a period of recovery. Recovery time and rehabilitation depends on the type of surgery performed. Physical therapy to help you regain strength in your hip and to restore range of motion, and this may include hydrotherapy. After your procedure, you may need to use a cane, crutches, or a walker for a time.
In most cases, surgery relieves the pain of osteoarthritis and makes it possible to perform daily activities more easily.
Finally, it is important to remember that healing after hip replacement surgery can continue for up to 12 months. Regular assessments with A/Prof Woodgate will ensure your best chance of an optimal outcome.