Osteotomy means "cutting of the bone." In a knee osteotomy, either the tibia (shinbone) or femur (thighbone) is cut and then reshaped or realigned to change the mechanical forces and relieve pressure on the knee joint.
Knee osteotomy is used when a patient has early-stage osteoarthritis that has damaged just one side/part of the knee joint. By transferring weight off the damaged side of the joint, an osteotomy can relieve pain and significantly improve function in an arthritic knee.
orthoinfo.aaos.org
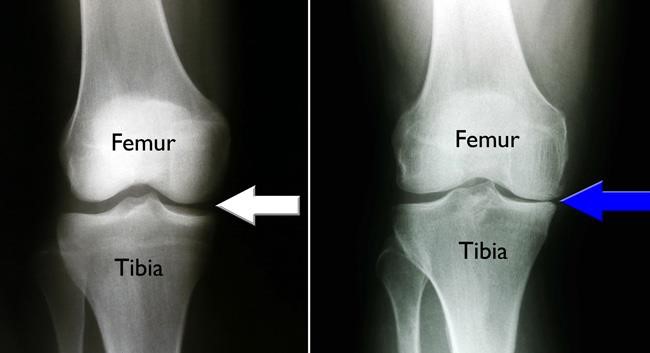
(Left) This x-ray of a healthy knee shows the normal joint space between the tibia and femur. (Right) In this x-ray, osteoarthritis has caused isolated damage to the inside portion of the knee. The tibia and femur are rubbing against each other, causing pain (blue arrow).
Advantages and Disadvantages
Knee osteotomy has three major goals:
- To transfer weight from the arthritic part of the knee to a healthier area
- To correct poor knee alignment
- To prolong the life span of the native knee joint
By preserving your own knee anatomy, a successful osteotomy may delay the need for a joint replacement for many years. Further, there are no restrictions on physical activities after an osteotomy - you will be able to participate in your favourite activities, even high-impact exercise.
Osteotomy does have disadvantages, including:
- Pain relief is not as predictable after osteotomy compared with a partial or total knee replacement.
- Recovery from osteotomy is typically longer and more difficult because you may not be able to bear weight on your operated knee right away whilst waiting for the bone to heal.
- In some cases, an osteotomy may make later knee replacement surgery more challenging, with potentially poorer outcomes.
Because results from total knee replacement and partial knee replacement have been so successful, knee osteotomy has become less common. Nevertheless, it remains an option for many patients.
Candidates for Knee Osteotomy
Knee osteotomy is most effective for thin, active patients who are less than 60 years old. Good candidates have pain on only one side of the knee, and no pain under the kneecap. Knee pain should be mostly activity-related or exacerbated by prolonged standing. Range of motion should be well maintained, and candidates should be able to fully straighten the knee and bend it at least 90 degrees. Patients with rheumatoid arthritis/inflammatory arthritis, or those with significant obesity are not good candidates for osteotomy.
Types of Knee Osteotomy
Knee osteotomies can be divided into 3 main types:
- High Tibial Osteotomy (HTO) – This procedure is usually done to correct bow-legged alignment/deformity, which is creating excessive stress on the inside of the knee, resulting in isolated medial (inner) knee arthritis. The aim is to transfer the forces to the uninvolved lateral (outer) part of the knee, which will create more space on the inner part and ease pressure in this area. It can be surgically done in one of three ways:
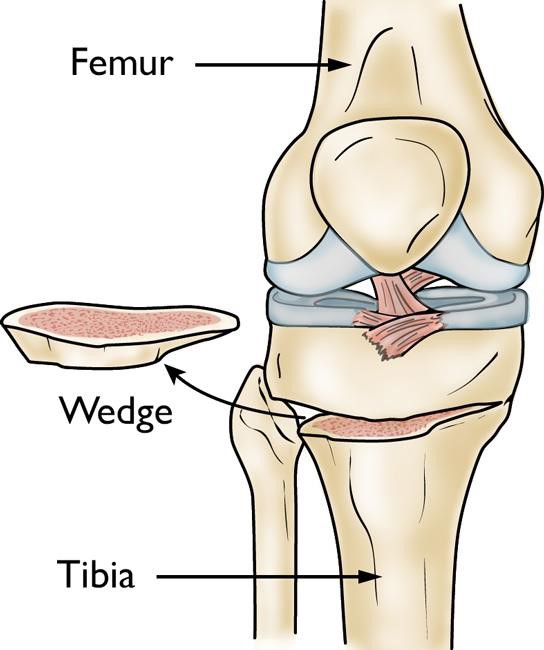
- Lateral “closing wedge” osteotomy involves removing a wedge of bone from the lateral (outer) side of the proximal tibia. After the remaining surfaces are brought together, a plate and screws (or staples) can be used to hold the position.
orthoinfo.aaos.org
In a tibial osteotomy, a wedge of bone is removed to straighten out the leg.
-
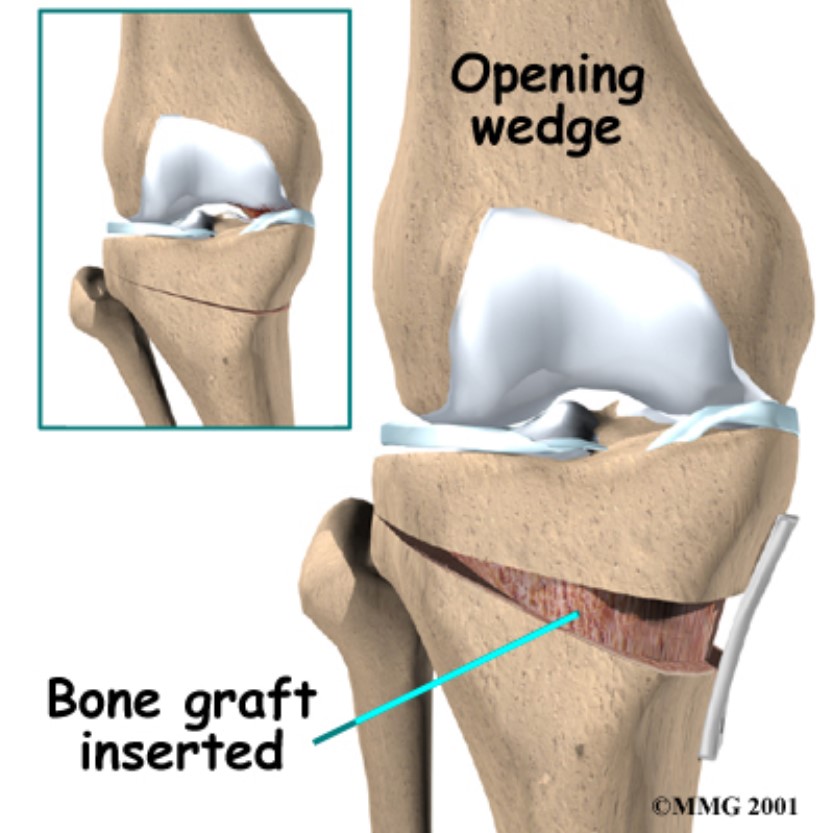
- Medial “opening wedge” osteotomy involves a cut in the proximal (upper) tibia, which is then levered open. Bone graft is inserted and a special plate is used to hold the gap until the bones heal.
orthoinfo.aaos.org
-
- Dome high tibial osteotomy requires a curved cut through the bone of the upper tibia, with the radius of the curve centred on the knee. The lower part is then rotated to the desired correction and fixed with a plate and screws. The advantage (theoretically) of this technique is that no bone is removed or required, which therefore does not effect the length of the leg, and the curved cut creates a larger surface area for improved healing.
- Distal Femoral Varising/Varus Osteotomy (DFVO) – This involves a cut through the lower end of the femur (thighbone) and this technique is mainly indicated for valgus (knock knee) deformity where there has been excessive stress to the lateral (outer) part of the knee. It also can be done with a “closing wedge’ technique, an “opening wedge” technique, or a dome technique, and subsequently fixed with a plate and screws. Interestingly, the results of DFBO have been somewhat better than those reported with HTO.
- Tibial Tubercle Osteotomy (TTO) – This involves cutting the bony insertion of the patellar ligament (also known as the patellar tendon) at the upper tibia and moving the insertion anteriorly (by placing a wedge of bone graft behind), medially (towards the inner part of the knee, or a combined anterior and medial shift. This technique is indicated when there is excessive anterior knee pain syndrome (shifting the kneecap tendon forwards decreases the overload on the kneecap), or for cases of patellofemoral (kneecap) maltracking with the aim of centering the patella in the grove of the lower femur. Occasionally, the TTO is done with lateral (outer) displacement to aid in exposure in revision knee replacement.
Risks and Complications
Possible risks and complications associated with knee osteotomy surgery include:
- Infection – This may occur in the superficial wound or deep around the fixation hardware. It may happen while in the hospital or after you go home, and may even occur years later. Minor infections in the wound area are generally treated with antibiotics. Major or deep infections may require more surgery and including washout or removal of the implants, though this may be delayed until the bone has healed.
- Blood clots (deep vein thrombosis) - Blood clots in the leg veins are one of the most common complications of knee surgery. These clots can be life-threatening if they break free and travel to your lungs (pulmonary embolism). A prevention program, which may include periodic elevation of your legs, lower leg exercises to increase circulation, compression (TED) stockings, calf compressors, early mobilisation, and medication to thin your blood (Clexane injections) is important. You will usually have a Duplex (ultrasound) scan of the lower leg veins 3-5 days post-surgery to look for any signs of DVT formation.
- Knee stiffness – This typically recovers over 6-12 weeks. It is more common in DFVO, and this is usually improved following delayed removal of the plate and screws.
- Nerve and blood vessel damage – This is rare, though most patients will report a persistent area of numbness to the lateral (outer) side of the surgical wound.
- Failure or delayed healing of the osteotomy – This may require revision surgery that can be combined with supplemental bone grafting.
- Over-correction or under-correction through the osteotomy
- Painful hardware
- Compartment syndrome – This is an increase in pressure in a muscle compartment that can impair or block the blood supply resulting in death and secondary scarring/contractures. It is more likely in HTO, and is prevented almost universally by the use of a wound drain. Early diagnosis within 4-6 hours is critical to prevent chronic muscle damage.
- Persistent pain in the affected area of the knee.
Recovery
Hospital discharge - In most cases, patients go home 2-4 days after an osteotomy.
Pain management - After surgery, you will naturally experience some pain. Many types of pain medication are available to help control pain, including opioids (including a PCA – Patient controlled analgesia system), non-steroidal anti-inflammatory drugs (NSAIDs) and local anaesthetics. Treating pain with medications can help you feel more comfortable, which will help your body heal faster and recover from surgery faster.
Weight bearing - After the operation, you will most likely need to use crutches for several weeks, until there are Xray signs of bone healing. A brace is used for protection while the bone heals. Weight-bearing on the leg is typically restricted, and you will be advised in each individual case.
Rehabilitation exercises - During rehabilitation, a physical therapist will give you exercises to help maintain range of motion in your knee and restore your strength, though certain exercises will be modified to prevent excessive stress on the fixation hardware until there is adequate bone healing.
Outcome
For most suitable patients, osteotomy is successful in relieving pain and delaying the progression of arthritis in the knee. It can allow a younger patient to lead a more active lifestyle for many years. Even though many patients will ultimately require a total knee replacement, an osteotomy can be an effective way to buy time until a replacement is required.
