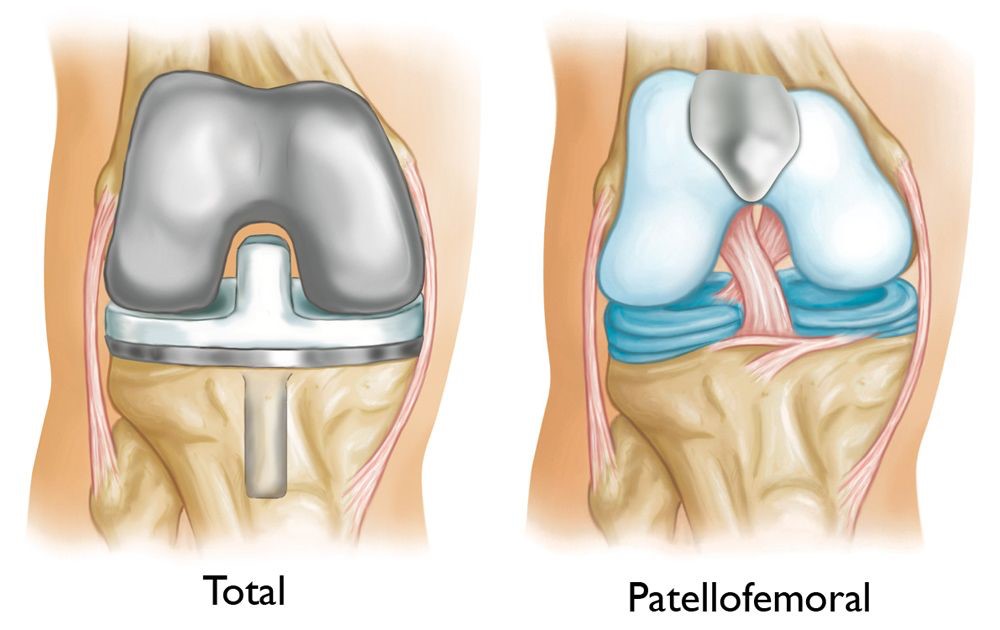
Patellofemoral replacement, also known as patellofemoral arthroplasty or kneecap replacement, is a type of partial knee replacement in which only a portion of the knee is resurfaced. The procedure is an alternative to total knee replacement for patients with isolated patellofemoral joint arthritis whose damaged bone and cartilage is limited to the underside of the patella (kneecap) and the channel-like groove (trochlea) in the femur (thighbone) in which the patella tracks. In this procedure the arthritic surface of patella (knee cap) is replaced with a highly cross- linked polyethylene (plastic) button and the corresponding articular trochlear surface on the distal femur is replaced with metal component. The healthy cartilage and bone, as well as all of the ligaments in the rest of the knee, are preserved.
Most of these patients are younger, and often it has been suggested to wait for total knee replacement until they are in their fifties or sixties despite the pain and disability of bone on bone arthritis.
Anatomy
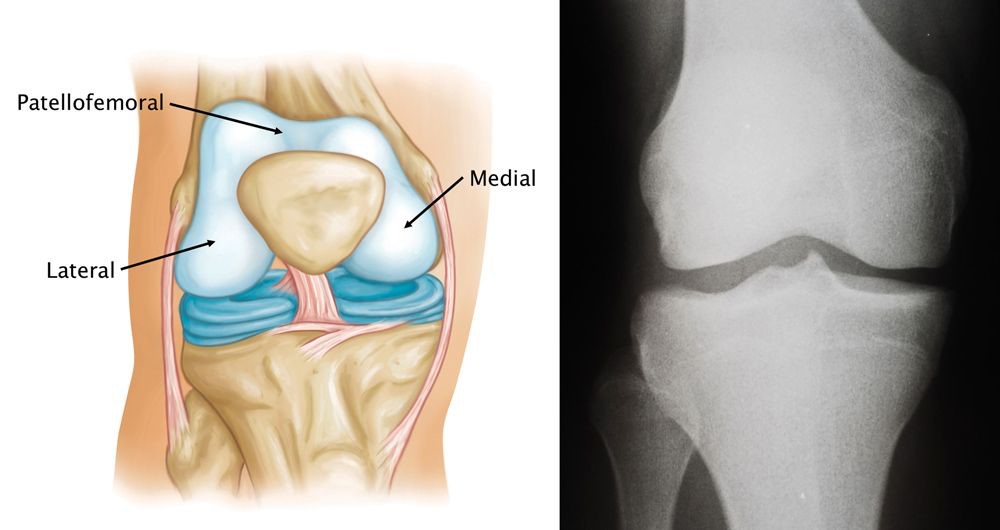
The knee joint is arbitrarily divided into three compartments for descriptive purposes:
- Medial compartment—the inside part of the knee
- Lateral compartment—the outside part of the knee
- Patellofemoral compartment—the front of the knee between the patella (kneecap) and femur (thighbone).
orthoinfo.aaos.org
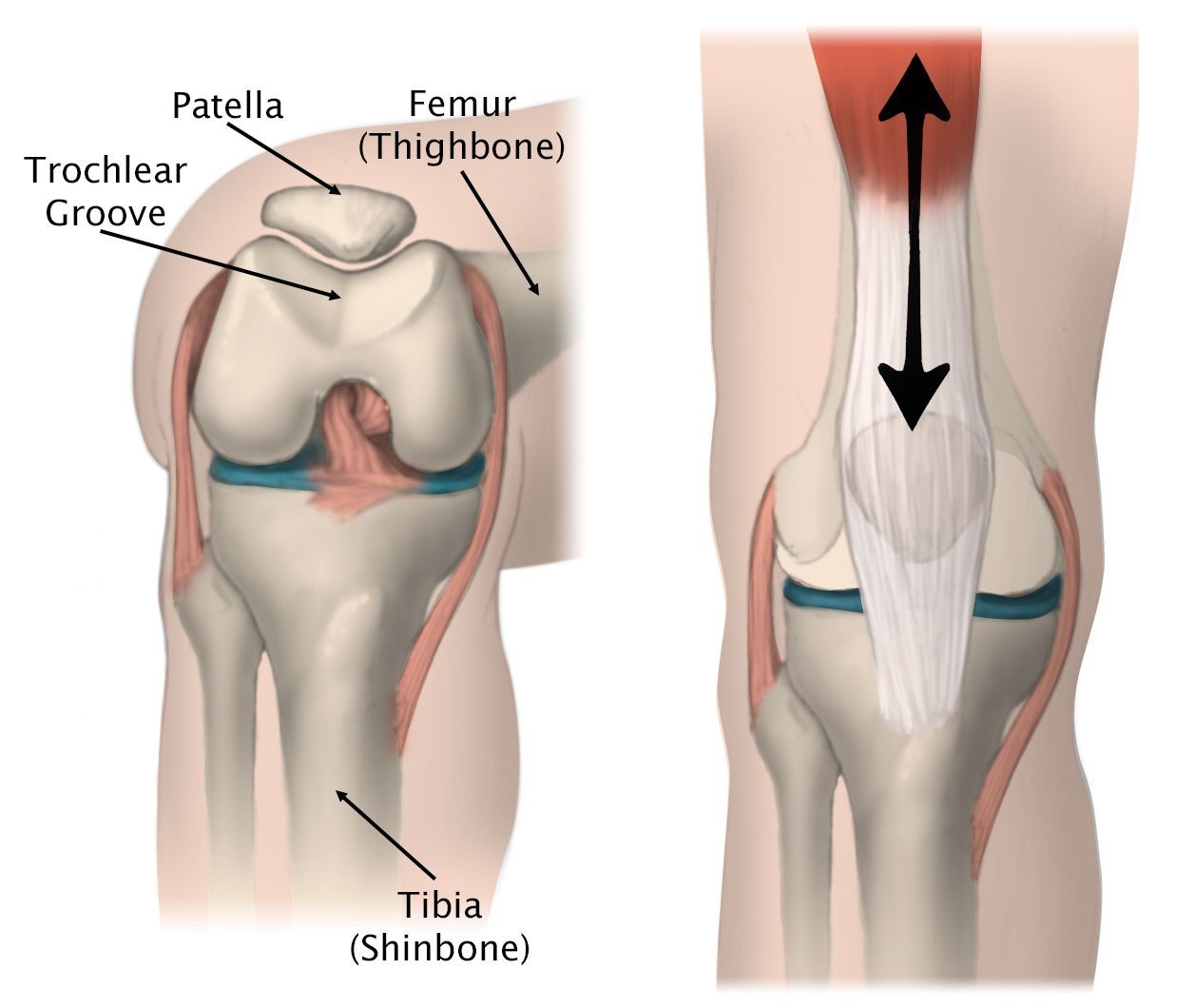
Within the patellofemoral compartment, the patella lies in a groove on the top of the femur called the trochlea. When you bend or straighten your knee, the patella moves up and down within this trochlear groove. Articular cartilage covers the ends of the femur, trochlear groove, the underside of the patella, and the upper surface of the tibia, and this allows movement of the joint.
orthoinfo.aaos.org
Patellofemoral Arthritis
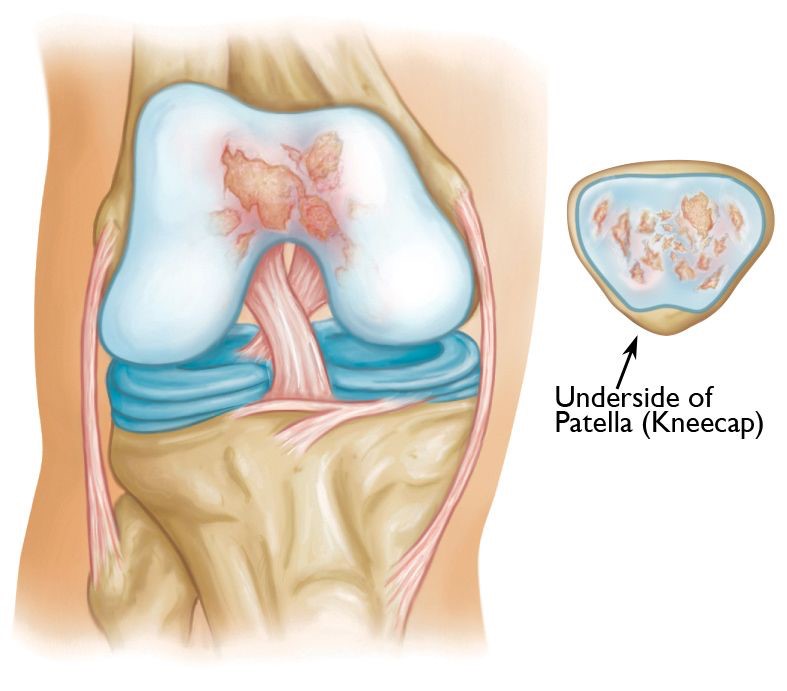
In patellofemoral osteoarthritis, the cartilage on the undersurface of patella and /or femoral trochlea wears away. The surfaces become more frayed, and underlying bone may become exposed, resulting in joint stiffness and pain. Moving the bones along this rough surface is painful. Patellofemoral joint arthritis occurs in isolation in less than 10% of patients with knee arthritis. The patients tend to be younger, with females much more commonly affected.
orthoinfo.aaos.org
Symptoms and Diagnosis
Patients with patellofemoral arthritis often present with symptoms of anterior knee pain (pain only behind the kneecap) that is worse with climbing or descending stairs, rising from a sitting position, and sitting for prolonged periods of time. A crunching or grinding sensation (crepitus) may be evident, along with some swelling and/or restricted knee range of motion.
Clinically, patients will often have tenderness around the patellofemoral region, often associated with signs of chronic patellofemoral maltracking. Signs of a ligamentous laxity syndrome are often found. Imaging studies used will include Xrays, MRI scans (to confirm the medial and lateral compartments are not involved), and occasionally CT scans.
Advantages of Patellofemoral Replacement
Potential advantages of patellofemoral replacement over a full total knee replacement include:
- Less blood loss
- Quicker recovery with earlier discharge from hospital
- Smaller surgical incision / less surgical trauma
- Decreased complications
- The functional and activity scores are better when compared to total knee replacement
- Many patients report that a patellofemoral replacement feels more natural than a total knee replacement, which is thought to be due to the fact that the bone, cartilage, and ligaments in the healthy parts of the knee are maintained.
orthoinf.aaos.org
An advantage of patellofemoral replacement over total knee replacement is that healthy parts of the knee are preserved, which helps to maintain more "natural" function of the knee.
Disadvantages of Patellofemoral Replacement
The major disadvantage of patellofemoral replacement compared with total knee replacement is the potential need for more surgery. Conversion or revision to a total knee replacement may be necessary in the future if arthritis develops in the other parts of the knee that have not been replaced.
Ideal Candidate for Patellofemoral Joint Replacement
The ideal patient for patellofemoral joint replacement is one with severe signs and symptoms of isolated patellofemoral compartment arthritis, correlated with X-ray proven arthritis, and with essentially no changes in the medial or lateral knee compartments (may need MRI scans to confirm), and for which nonsurgical treatment options are no longer giving adequate relief of symptoms.
You may not be a good candidate for the procedure if any of the following characteristics are present:
- Knee stiffness
- Ligament damage
- Major deformity of the leg
- Inflammatory arthritis (such as rheumatoid arthritis)
- Crystalline arthritis (such as gout)
- Morbid obesity.
Surgical Procedure
The surgery is usually performed under spinal and/or general anaesthesia, combined with intraoperative injections of local anaesthesia into the wound. A femoral nerve sheath catheter is inserted by the anaesthetist at the end of the surgery and connected to a "Pain buster" local anaesthetic infusion device, which typically runs for about 48 hours.
A/Prof Woodgate performs a diagnostic knee arthroscopy for all the patients before the actual skin incision to confirm suitability for the procedure, that is, isolated patellofemoral arthritis and rest of the knee is essentially normal. If damaged cartilage is found in other areas of the knee, the patellofemoral arthroplasty is not performed. A contingency plan will have been discussed with you prior to surgery to make sure that you agree with alternative strategies, either arthroscopic debridement or a total knee replacement.
An incision is made over the front of the knee incorporating the knee arthroscopy wound, and the distal femur and patella are exposed. The wound is smaller than the normal incision for total knee replacement. Specialized surgical guides are used to remove the worn-out surface under the patella and to shape the trochlear groove of the femur. The metal component, similar in size and shape to the end of the femur, is cemented to the bone. and the patellar button is also cemented.
Once the components are inserted, the knee is moved along the range of motion to confirm the accurate positioning and tracking of the implants. The wound is closed in layers over a suction drain. The operation takes about 60-90 minutes to complete. A/Prof Woodgate utilises the RBK Patellofemoral Joint System for this procedure.

orthoinfo.aaos.org

smw.ch
Post-Operative Care and Management
- After surgery, you will be taken to the recovery unit where you will be closely monitored until you recover from the anaesthesia, and this time is variable. Pain relief will be provided as needed. Once your condition is assessed as stable, transfer to the Orthopaedic ward will occur.
- A large dressing will cover the surgical wound on the knee, and this extends from your thigh to your ankle. There will also be a knee immobilizer (splint) in place over the dressing.
- Under the dressing and resting in the wound is the suction drain, which is usually removed on day 1 post surgery
- The following morning (day 1), the physiotherapist will assist you with mobilisation, initially with the help of a walking frame and commence an exercise protocol.
- The knee splint is used while walking for first few days, and until the dressings are lightened on day 2, at which time you should be able to perform a straight leg lift in the bed.
- Sterile waterproof adherent dressings are applied to the surgical site on day 2 after the bulky dressing is taken down, and long TED stockings are worn (for 6 weeks).
- The physiotherapist will progress your mobilisation to become more independent, from the walking frame to crutches and then to a cane.
Discharge from Hospital
- Most patients will be safe for discharge after 3-5 days, though some patients elect to be transferred to an inpatient rehab facility to fast track their early exercise programme.
- The knee waterproof dressing remains intact for 7-10 days, at which time it may be left off, except when undertaking hydrotherapy.
- Long TED stockings will continue to be used for 6 weeks.
- Medications and analgesics will be prescribed at discharge, and this may also include blood-thinning injections (Clexane).
- It is important to use ice packs regularly (for 20 minutes every 2 hours) to decrease swelling in the knee.
- A follow-up appointment will be given to see A/Prof Woodgate at 2 weeks post surgery.
- Any bruising noted around the thigh and knee extending to the shin and lower leg typically resolves over 10-14 days, though some swelling and warmth may still be noted.
If any increasing pain, swelling, redness, or fever develop, it is very important to contact A/Prof Woodgate as soon as possible.
Expectations and Outcomes
The majority of patients will expect to progress as follows:
- For the first 2 weeks after surgery, your activity level may be limited, but you should be able to walk independently (perhaps with the assistance of a cane) and use bathroom and kitchen facilities.
- After 2 weeks, climbing stairs usually becomes easier, though descending still may require the assistance of the railing.
- By 6 weeks, most normal everyday activities should have resumed, though squatting down may take some time.
- Complete wound healing takes about 6 to 8 weeks. During this time, some swelling and discomfort is normal and should be manageable with the prescribed medications and regular use of ice packs and the long TED compression stockings.
- An occasional patient may require an injection of cortisone (after 12 weeks) to relieve tissue soreness due to surgery and readjustment of the knee.
- Some patients may experience a small area of numbness on the lateral aspect (outside edge) of the incision. This may or may not resolve over time and can take 6 to 12 months.
- Most patients report ongoing improvement for 6-12 months, and it is important to continue a regular knee exercise programme.
Complications
As with any surgical procedure, there are risks associated with patellofemoral replacement. These risks are similar to those of total knee replacement. A/Prof Woodgate will discuss the risks with you and will take specific measures to help avoid potential complications.
The possible risks of patellofemoral replacement include:
- Infection
- Blood clots (DVT)
- Persistent pain
- Patellar instability (dislocating kneecap)
- Injury to surrounding structures, including blood vessels or nerves
- Reaction to anaesthesia
- The need for additional surgery, especially if arthritis progresses in the rest of the knee.
