Definition
A malignant tumour of cartilage producing cells.
A secondary chondrosarcoma arises in a benign cartilaginous tumor, most commonly in osteochondromas particularly in the multiple, familial type.
Dedifferentiated chondrosarcomas are chondrosarcomas that have given rise to more highly malignant tumours such as osteosarcomas, fibrosarcomas and MFH.
Incidence
60 in NSW 1991-1995 (i.e 10-12 cases per year), making up 25% of all primary malignant bone tumours.
In the Mayo data chondrosarcoma is less frequent making up about 9.2% of malignant tumours, and chondrosarcoma occurred half as often as osteosarcoma.
The Nov 2001 CCR says chondrosarcoma is the third most common bone tumour after osteosarcoma (OS) and Ewing’s sarcoma (ES).
There is a slight male predominance.
They are primarily tumours of adulthood and old age, except for secondary chondrosarcoma that tends to occur earlier.
Localization
2/3 of the tumours are in the trunk and upper ends of the femur and humerus
The most common sites are the pelvis (24%) and the proximal part of the femur (16%).
It is remarkably rare in the distal portions of the limbs, with only about 2% occurring distal to the ankles and wrists. It is also rare in the spine. If it involves the spine, the posterior elements are affected.
The metaphysis is the most common part of the bone affected, but there may be extension into the epiphysis.
Classification
1. By grade
- Atypical enchondroma (grade ½ chondrosarcoma) or atypical chondromatous lesion. This is a premalignant or borderline lesion
- Low-grade (Grade 1)
- Medium-grade (Grade 2)
- High-grade (Grade 3)
The higher the grade the more likely it is that the tumour will metastasize.
2. Primary or secondary
- Primary lesions arise de novo
- Secondary chondrosarcomas arise in a pre-existing benign cartilage lesion which can be an enchondroma, an osteochondroma, a chondromyxoid fibroma, synovial chondromatosis, a periosteal chondroma or a chondroblastoma
i. Patients with Ollier’s disease have about a 25% risk of developing chondrosarcoma.
ii. Patients with Maffucci’s syndrome have an extremely high risk, with Schwartz predicting a lifetime incidence of 100% (including other tumours - intrapelvic and intraabdominal).
3. Central or peripheral
- Central chondrosarcoma arises from within the medullary canal
i. Primary chondrosarcomas are almost always central - Peripheral chondrosarcomas arise from the surface of the bone
i. Most are secondary to an osteochondroma
ii. In distinguishing between periosteal chondromas and periosteal chondrosarcomas the size of the tumour is important. Periosteal chondromas are usually less than 3cm in size and periosteal chondrosarcomas are usually more than 5cm in size. A cartilage cap of more than 2cm is indicative of malignancy (Nov 2001 CCR)
4. Specific histological subtypes
- Clear cell
i. This is thought to be the malignant counterpart of a benign chondroblastoma
ii. Most common in the proximal part of the humerus and the proximal part of the femur – involves epiphysis. This can create confusion with chondroblastoma
iii. Occur in younger patients, from 20-50 and are more common in men
iv. Usually low grade, have a much better prognosis than central chondrosarcoma. - Mesenchymal
i. Comprises nodules of benign appearing cartilage within a background of undifferentiated small round cells
ii. Has a poor long term prognosis - Soft parts
i. This is the term for a chondrosarcoma arising in soft tissues
ii. It is very rare and little is known about its natural history - Dedifferentiated
i. When a benign or low-grade chondrosarcoma transforms into a highly malignant variety of sarcoma eg osteosarcoma, MFH. The diagnosis is made when both the low and high grade lesion are found together on histology. The prognosis is very poor.
Pathology
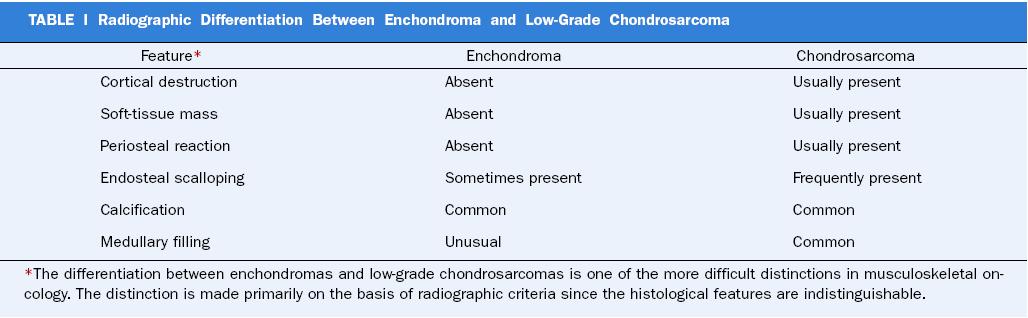
It is very difficult to distinguish between a low-grade chondrosarcoma and an enchondroma.
Generous material to study is mandatory. Because of the similarity, clinical and radiographic criteria must be used to separate a benign enchondroma from a low-grade malignant cartilaginous neoplasm
The best distinguishing feature is the permeative quality of chondrosarcoma; it tends to wrap around and entrap bony trabeculae. An enchondroma has a bone encasement pattern. Enchondroma = Encasement
Molecular biology
t(9;22) translocation is found in 25%.
Grading
Mitotic features are very rare in chondrosarcomas - they are found in only six percent.
Therefore the characteristics that are used to grade chondrosarcomas are the cellularity of the neoplasm and the cytological atypia.
61% of tumors are grade 1
36% are grade 2
Only 3% are grade 3
Recurrence
Recurrent tumours have an increase in grading in around 10%.
Dedifferentiated chondrosarcoma
Has areas of malignant spindle cells that cannot be recognized as being of cartilaginous origin, adjacent to areas of neoplastic chondrocytes surrounded by a hyaline-cartilage matrix.
Clinical
Local swelling and pain. Chondrosarcoma’s are almost always associated with pain, whereas enchondromas rarely are.
As in other bone tumours the characteristics of the pain and swelling offer little help in diagnosis, although there is a prolonged course that may offer a clue.
The slow clinical course is emphasized by the fact that there may a 5-10 year interval or even more between treatment and recurrence.
Recurrence is common, with a figure of 26.5% at 10 years reported at the Mayo Clinic
Metastasis is rare and often occurs late. It is almost always to the lungs.
Laboratory studies
The ESR may be elevated but this is uncommon.
There are no other abnormalities
Radiology
Chondrosarcomas tend to be large.
Small lesions tend to be round or oval.
Large lesions have a marked tendency to conform to the shape of the bone.
There is often cortical expansion and cortical thickening. Scalloping of the endosteal cortex is a sign of malignancy.
Matrix mineralization is common but 25% of tumours don’t show it. The calcification is best seen on CTs.
40% of tumours have an associated soft tissue mass. This is best demonstrated on MRIs. Note: on T2 weighted images the cartilage has a high signal.
The development of a thickened cartilaginous cap (>2cm) is a sign of malignant transformation from an osteocartilaginous exostosis to a secondary chondrosarcoma.
Treatment
The treatment of chondrosarcoma is primarily surgical, since the response to chemotherapy and radiotherapy is relatively low.
The basic therapeutic goal is to control the lesion locally and prevent recurrence.
The optimal surgical strategy is early surgical removal with a wide margin of uninvolved tissue. The tumour should be excised completely so that the surgeon doesn’t break into or see the tumour at any time. If possible, an open biopsy will be examined immediately by frozen section. Ideally, the resection will proceed immediately after confirmation of the diagnosis, at the same procedure.
In chondrosarcomas secondary to osteochondromas a wide/marginal excision is satisfactory in most cases. In most cases this will be an excisional biopsy.
Chemotherapy and radiotherapy are ineffective.
Types of pelvic resection for limb salvage
Limb salvage is thought feasible in patients with pelvic chondrosarcoma if two of three structures comprising the hip joint, femoral neurovascular bundle and lumbosacral plexus were thought to be preservable. If adequate margins or the above conditions can’t be met a hemipelvectomy is performed.
Type I - includes only the ilium
Type IA - includes the ilium and gluteal muscles
Type I/S - includes the ilium and sacro-iliac joint
Type II - periacetabular resection
Type IIA - includes the hip joint
Type III - resection of all or a portion of ischium and pubis
Prognosis
- 5-year survival rates are not very significant as a criterion for cure because of the high recurrence rate. 10-year survival rates are more representative. The overall five-year survival rates are around 70-80% and 10-year survival rates are around 50-66%. The rates are worse in pelvic chondrosarcomas and there is a higher rate of recurrence. In the 2001 Mayo series of pelvic chondrosarcomas the recurrence rate was 19%.
- Childhood chondrosarcoma has the same prognosis as adult chondrosarcoma.
- Chondrosarcomas arising from osteocartilaginous exostoses have a better prognosis than other chondrosarcomas and these lesions rarely metastasize. However, they may turn into de-differentiated chondrosarcomas. The development of a thickened cartilaginous cap (>2cm) is a sign of malignant transformation from an osteocartilaginous exostosis to a secondary chondrosarcoma.
- Dedifferentiated chondrosarcoma has a terrible prognosis with a 5-year survival rate of 10%.