Pathophysiology
- Source of primary low back pain &/or lower extremity pain in approximately 15-30% of patients with low back pain
- Idiopathic
- Extra-articular:
- Enthesis / ligamentous sprain
- Insufficiency fracture
- Fracture after major trauma
- Possible predisposition with ligamentous laxity conditions
- Intra-articular:
- Osteoarthritis
- Infection
- Usually haematogenous spread & unilateral
- Occasionally iatrogenic, e.g post injection
- Pseudomonas aeruginosa, Staphylococcus aureus, Cryptococcus, Mycobacterium tuberculosis
- Predisposing factors include trauma, endocarditis, IVDU, & immunosuppression
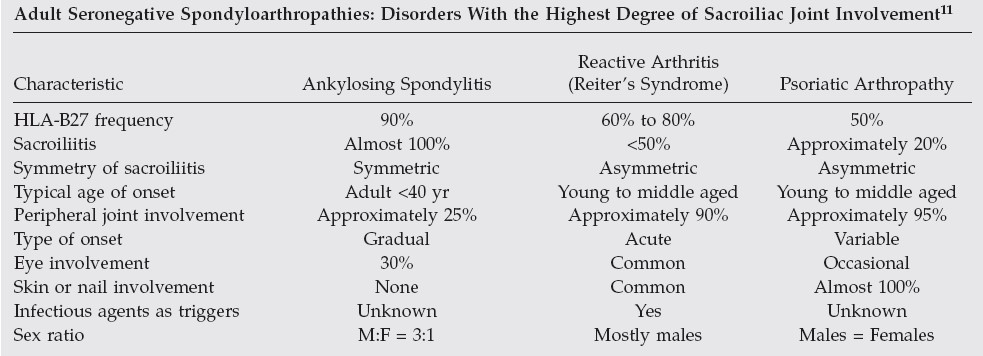
- Inflammatory arthropathies
- Ankylosing spondylitis
- Reiter’s syndrome
- Psoriatic arthropathy
-
- Metabolic processes
- CPPD disease
- Gout
- Ochronosis
- Hyperparathyroidism
- Renal osteodystrophy
- Acromegaly
- Tumours
- GCT
- Chondrosarcoma
- Synovial villoadenoma
- Metastases
- Instability
- Iatrogenic (overzealous bone harvesting for grafts or from pelvic resection of tumours)
- Pregnancy
- Typically 3rd trimester of pregnancy results in hypermobility of sacroiliac joint because of increased levels of estrogen & relaxin that cause soft tissues supporting joint to loosen – pain can develop earlier in some patients
- This laxity may predispose sacroiliac joint ligaments to painful sprain
- Mechanical trauma of childbirth also may cause joint pain
- Lumbar spine fusion or hip arthrodesis may transfer additional forces to sacroiliac joint, creating cumulative stress and pain (43% of patients develop some level of sacroiliac degeneration within 5 years of lumbar fusion)
- Metabolic processes
Differential Diagnosis
- Intrinsic disk disease
- Nerve root compression
- Zygapophyseal joint pain
- Primary or secondary myofascial syndromes
- Non-spinal structures:
- Gastrointestinal
- Genitourinary
- Gynecologic
- Hip joint dysfunction
Diagnostic evaluation
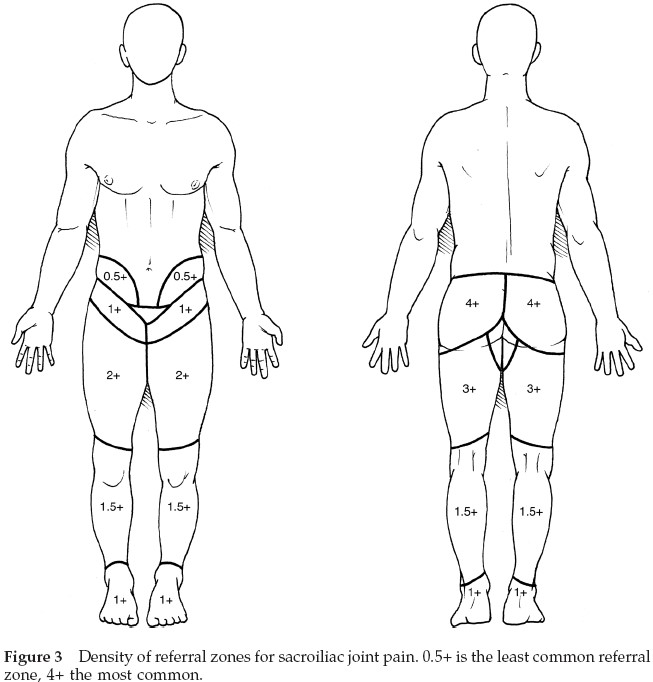
- Pain patterns:
- Referred pain to an area just inferior to ipsilateral PSIS
- Physical examination:
- Used to exclude other diagnostic possibilities
- A false-positive straight leg raise test may occur when affected leg is elevated to approximately 60° because false dural tension symptoms are caused by sacroiliac joint motion at this degree of elevation
- Imaging:
- Plain radiographs
- AP pelvic & inlet & outlet views, and sacroiliac views +/- lateral sacrum
- When instability suspected; single leg weight-bearing pelvic (flamingo) views
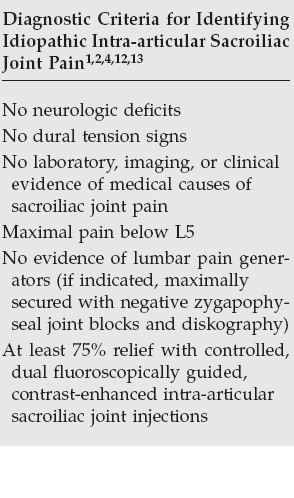
- CT, MRI, & bone scan may be done predominantly to exclude other causes of pain rather than to diagnose idiopathic sacroiliac joint pain
- Plain radiographs
- Diagnostic injections:
- Fluoroscopically or CT-guided, contrast-enhanced injections
- Maximum volume that should be injected into sacroiliac joint is 2.5 mL
- Excessive injectate can leak from anterior capsule onto regional neural structures & limit diagnostic specificity
Management
- Medications:
- NSAIDs
- Non-opiate analgesics
- Opiates
- Anti-depressants
- Adjunctive medication including protease & TNF inhibitors
- Last 3 in liaison with rheumatologist & pain unit
- Physical therapy:
- Education in & training of proper body mechanics & posture are essential, as is aerobic conditioning
- Flexibility & strength training (hamstrings, gluteus maximus & medius, piriformis, erector spinae, latissimus dorsi, & iliacus muscles)
- Avoid excessive hip external rotation and “clam” exercises
- Braces (pelvic belt):
- May provide some pain relief &/or proprioceptive feedback
- Rapid weaning avoids psychological dependence & prevents decreased soft-tissue flexibility & potential muscular weakness
- Injections (corticosteroid):
- Following minimum 4 weeks of appropriate, directed, noninvasive conservative care
- If pain substantially inhibits work or progress in physical &/or manual therapy, earlier use of an injection procedure may be diagnostic & may provide therapeutic benefit
- Prolotherapy Injections:
- 3 separate image-guided intra-articular (+/- extra-articular) injections of 50% Dextrose, each injection given 3-4 weeks apart
- Reported to give benefit in 75-80% of patients
- Less successful if associated with ligamentous laxity syndrome
- Radiofrequency neurotomy:
- Indicated after other, less invasive methods of care have been exhausted & diagnosis is proven for chronic joint pain
- L5 dorsal ramus, its branches to sacroiliac joint, & lateral branches of S1-S3 dorsal rami
- More effective for extra-articular than intra-articular joint pain
- 65% report >50% reduction of pain at 6-month follow-up
- Arthrodesis:
- Considered only in patients with joint pain proven by controlled diagnostic anesthetic blocks & without any pain sources in lumbar spine
- It also should be reserved for those who continue to have disabling symptoms that have not responded to aggressive conservative care, i.e. failed non-operative programme
- Procedures
- Anterior approach – Open ilioinguinal exposure with joint debridement, bone graft, and double-plate fixation – best for significant instability +/- ligamentous laxity patients
- Posterior – Minimally invasive extra-articular approach using DIANA (Distraction Interference Arthrodesis with Neurovascular Anticipation) technique – Should not be used for ligamentous laxity patients
- Direct Lateral/Transgluteal – Minimally invasive technique using iFuse 3D (better than original iFuse as allows extra bone graft) – Also quicker rehab protocol
- Stabilisation with transiliosacral screws not recommended except in the acute trauma situation
- Post-operative care
- PWB 3-12 weeks, depending on technique
- Serial Xrays to confirm fixation and progressive union/fusion
- CT to confirm consolidation in DIANA cases at 3 and 6 months
