Introduction
-
Acute low back pain:
- Defined as low back pain lasting up to 12 weeks
- Most common between ages 35 to 55 years
- 60 to 70% severe enough to require work absence return to work within 6 weeks; 80% to 90% return within 12 weeks
- 70 to 90% of patients will have improvement in back pain within 1st month after onset regardless of treatment
- Recurrence 20 to 72%
- Chronic low back pain:
- Definition
- Low back pain lasting longer than 12 weeks; or
- Frequently recurring low back pain; or
- Pain lasting beyond normal healing period for a low back injury
- Chronic symptoms develop from an acute episode in 5 to 10%
- Definition
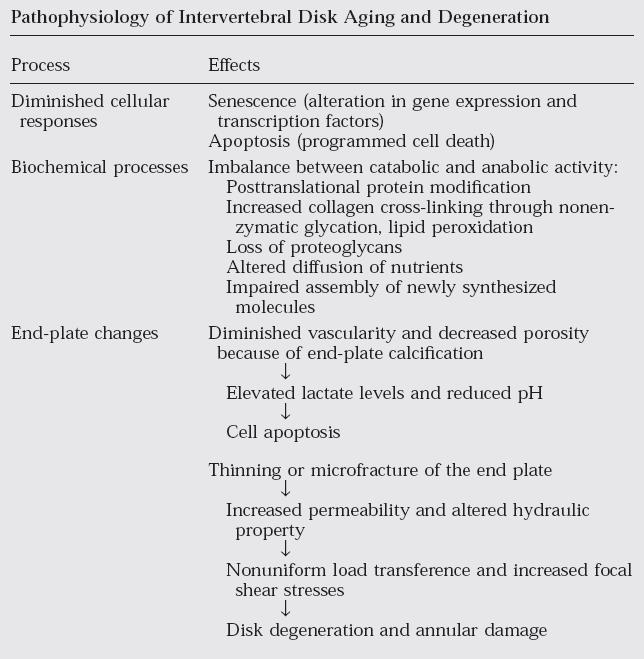
- Pathophysiology:
- Clinical manifestations:
- Symptoms usually develop subsequent to an accident or incident, but often onset is insidious
- Pain typically increases with activity & decreases with rest
- Imaging:
- Demonstrate either no abnormalities or varying degrees of degenerative changes, which often are those that are expected as part of normal aging
- Disorders of cauda equina &/or lumbar nerve roots:
- Distinguished from more common type of back pain by the presence of radicular symptoms with or without neurologic changes
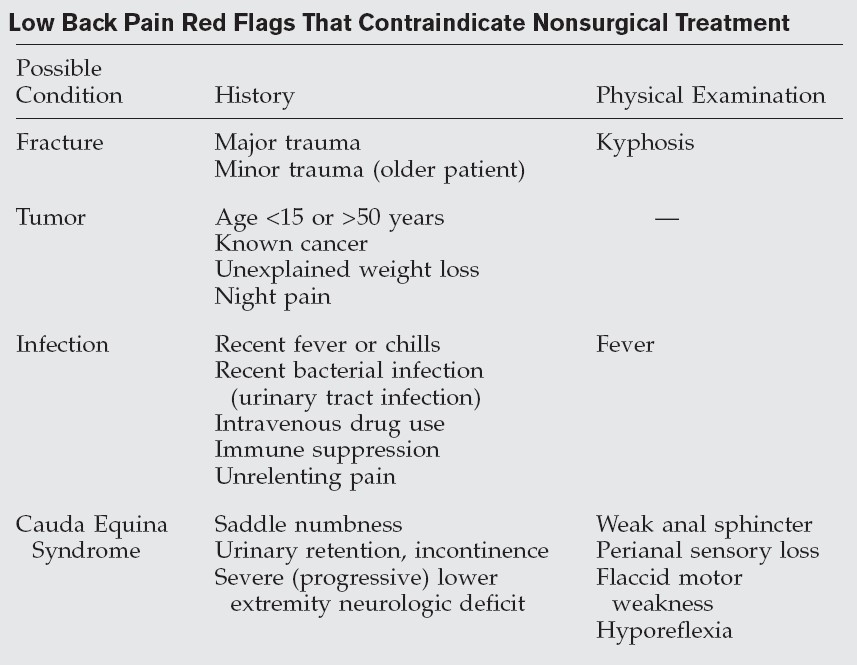
- Non-musculoskeletal aetiology of low back pain:
- Renal
- Calculi
- Infection
- Tumour
- Vascular
- AAA
- Renal
Non-operative Management
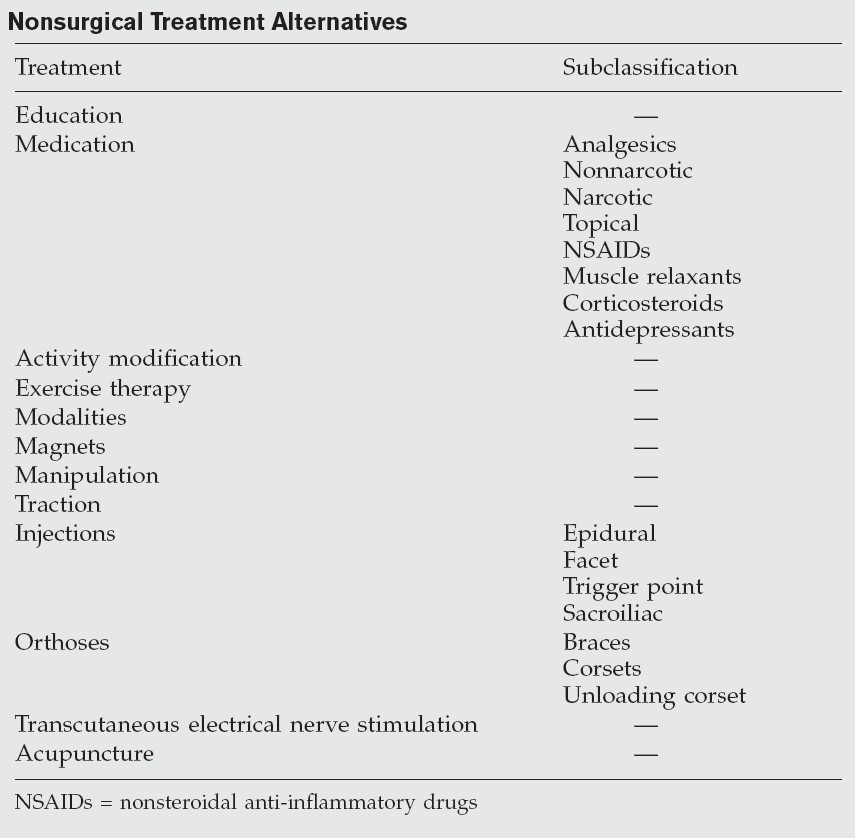
- Education:
- Expected outcome & favourable natural history of low back pain
- Assist them to become active participants in their own treatment
- Correct posture & lifelong commitment
- Prevention of dependence on medication
- Medication:
- Non-narcotic analgesics
- Acetaminophen (paracetamol)
- ® Mild to moderate pain
- Highest dose in adults is 4 g/day
- Prolonged high-doses can result in severe or fatal hepatotoxicity (LFTs if taken for > several months)
- ® Should be avoided in patients who abuse alcohol or have a known hereditary liver disease
- Tramadol
- ® Centrally acting analgesic chemically unrelated to opiates
- Weak effect on monoamine oxidase receptors in spinal cord & competes with narcotics; thus, tramadol should not be used concurrently with opioids
- Should be used cautiously in patients taking monoamine oxidase inhibitors because tramadol inhibits noradrenaline & serotonin uptake
- Dosage reduction recommended in patients with impaired hepatic or renal function & in persons > 75 years
- Short-term use recommended & reserved for patients with severe pain
- Acetaminophen (paracetamol)
- Narcotic analgesics
- Only in patients whose pain is unresponsive to appropriately prescribed alternative medications or when other analgesics are contraindicated
- Short-term
- Topical analgesics
- Capsaicin induces & depletes substance P from sensory C-afferent nociceptive nerve fibres
- May be useful for mild pain
- NSAIDs
- Inhibit synthesis of enzyme cyclooxygenase (COX), thus inhibiting synthesis of prostaglandins
- Celecoxib (Celebrex) decreased gastrointestinal side effects due to selective action on COX-2
- Muscle relaxants
- Short-term management of acute back pain
- Side effects include abuse potential, dependence, withdrawal when abruptly discontinued, drowsiness, & dizziness (later 2 may be reduced by night-time administration)
- Oral corticosteroids
- Short-term use in patients with radiculopathy
- Potential for severe side effects associated with either long-term use or with short-term use in high doses (>60 mg) limits use as a first-line agent & precludes use with chronic low back pain
- Antidepressants
- Tricyclic antidepressants (e.g. amitriptyline)
- Neurogenic pain, in particular chronic back pain & chronic pain syndromes
- Sleep disturbance is not uncommon in patients with chronic low back pain & is often related to depression
- Sedative properties & therefore recommended for night-time use
- Neuropathic modification
- Pregabalin (Lyrica) and Gabapentin
- Non-narcotic analgesics
- Activity modification:
- Bed rest for maximum of 48 hours following an acute episode
- Painful activities should be avoided for at least a few days until more acute symptoms decrease then encouraged to remain physically active
- Fear-avoidance beliefs about work & physical activity (i.e. avoidance of work & activities because of fear of increased symptoms) are strongly related to disability caused by back pain
- Passive physical therapy:
- Cold packs
- Cold provides pain relief & reduces inflammatory response by vasoconstriction following an acute injury
- Heat packs
- Heat relaxes muscles, improves tolerance to exercise, & may be a reasonable modality when acute phase is over (after 1 to 2 weeks)
- Massage therapy
- Subacute & chronic back pain
- Cold packs
- Exercise therapy:
- Low-impact cardiovascular & aerobic exercises provide other benefits, such as improved mood, increased pain tolerance, & prevention of deconditioning
- Low-stress aerobic exercises can be started during 1st 2 weeks after onset of low back pain symptoms
- Trunk stabilisation & muscle strengthening exercises useful for chronic low back pain, restoring normal lumbosacral motion & emphasise correct body mechanics & posture
- Reduce risk of bone demineralisation & associated fragility fractures
- Magnets:
- No benefit demonstrated in controlled trials
- Manipulation:
- Include chiropractic & osteopathic modalities (no strong supportive data)
- May reduce symptoms in 1st 6 weeks
- Should be discontinued & patients reassessed when symptoms persist or when there is evidence of radicular neurologic symptoms
- Once acute episode resolved, no evidence supports practice of maintenance treatments
- Severe or progressive neurologic deficits are contraindications to manipulation
- Traction:
- No high-quality RCTs demonstrate a benefit
- May be generally associated with a greater morbidity, especially in elderly
- Injections:
- Epidural corticosteroids
- Interlaminar, caudal, & transforaminal methods
- Fluoroscopy to reduce complications & misplacement
- Effective in patients with radiculopathy
- No evidence that they are effective for acute low back pain
- Strong evidence for use in chronic low back pain
- Complications include dural puncture, spinal cord injury, epidural haematoma, abscess formation, & nerve damage
- Limited to no more than 3 in a 6-12 month period
- Not appropriate when there is no indication of radicular nerve–related symptoms
- Facet joint
- Facet joint osteoarthritis
- No evidence supports use in management of acute low back pain, however may provide short-term functional improvement in patients with chronic low back pain
- Intra-articular, medial branch blocks & medial branch neurolysis
- Facet joints are richly innervated by branches from posterior primary rami
- Denervation needs to consider direct, local, & ascending facet branches
- Overlapping nature of innervation means that to denervate 1 segment effectively, 3 levels may have to be approached
- Radiofrequency neurotomy (rhizolysis) has also been found to provide short-term relief of chronic low back pain
- ® Should be considered only after multiple facet blocks have been performed
- Trigger point
- May be useful in back pain secondary to myofascial syndrome
- Sacroiliac joint
- Diagnostic, to exclude alternative source of pain – 15-30% of back pain reported to originate from sacroiliac joint
- Prolotherapy
- Involves injections with sclerosing agents into ligaments of back & pelvis
- No scientific evidence supporting its efficacy in facet disease – some good reports with sacroiliac pathology
- Epidural corticosteroids
- Orthoses:
- No direct evidence however may act as proprioceptive reminders to use correct spine mechanics during lifting & bending activities
- Transcutaneous electrical nerve stimulation (TENS):
- Short-term relief
- Acupuncture:
- Literature demonstrates mixed results
- Behavioural therapy:
- Includes cognitive behavioural therapy
- Enhance treatment by addressing cognitive (negative emotions & thoughts) & behavioural (altered activity & medication dependence) aspects of chronic pain
