Introduction
- Symptoms typically develop between 50 to 60 years of age in association with lumbar spine osteoarthritic changes
- No sex predominance, although degenerative spondylolisthesis associated with lumbar spinal stenosis 4x more common among women
- No association found with occupation or body habitus
- Usually caused by a reduction in space available for neural elements due to variant osseous anatomy or filling of spinal canal with hypertrophic tissue
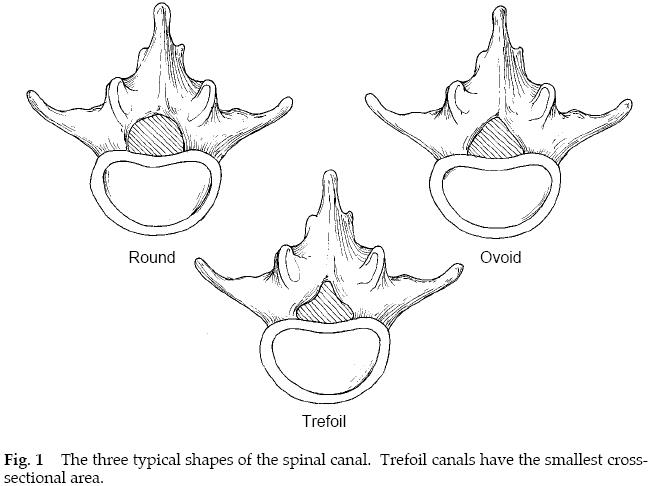
- Central stenosis:
- Compression of dural sac is main component
- <10mm canal AP diameter or 100mm2 canal cross-sectional area on CT
- Lateral stenosis:
- Compression of nerve root in lateral recess, neural foramen, or lateral to neural foramen
Pathophysiology
- Usually begins with disk dehydration, resulting in a loss of disk height & bulging of annulus fibrosus & ligamentum flavum into spinal canal
- These changes alter loading of facet joints, which together with intervertebral disc form 3-joint spinal motion segment
- Further degeneration leads to facet arthrosis with sclerosis & osteophytic overgrowth
- Most common result is as nerve roots traverse lateral recesses, they are encroached on by hypertrophic facet joints, infolded ligamentum flavum, & a bulging annulus
- These degenerative changes can also cause root stenosis in neural foramen
- AP diameter of foramen is reduced by bulging anulus anteriorly & hypertrophic facets posteriorly, while foraminal height is reduced by loss of intervertebral disc height & associated facet subluxation
- Degenerative process is sometimes accompanied by development of segmental instability
- Degenerative changes in supporting structures of spinal motion segment, including compromise of facet joints & capsular ligaments, may cause higher mechanical stress across degenerated annulus, leading to development of dynamic subluxation or spondylolisthesis
- As abnormal motion develops within a degenerated motion segment, it exacerbates nerve root irritation in stenotic lateral recess & foramen
Clinical Manifestations
- History:
- Insidious onset & a slow rate of lumbar back pain with progression to lower-extremity pain
- Neurogenic claudication
- Exacerbated by standing, walking, & exercising in an erect posture, which results in development of pain, tightness, heaviness, & subjective weakness in legs
- Relieved by sitting down or leaning forward
- Activities in which lumbar spine is in flexion, such as walking uphill, leaning forward on a walker or shopping cart, or riding a bicycle, are usually better tolerated
- Motor, gait, bowel & bladder dysfunction uncommon
- Examination:
- Lumbar lordosis reduced with ROM diminished
- Deep tendon reflexes diminished with complete loss in elderly common
Differential Diagnosis
- · Vascular claudication:
- Reproduced at a consistent level of exertion (e.g. walking 2 blocks)
- · Diabetic neuropathy:
- Characterised by a stocking-glove distribution
Imaging
- Erect plain radiographs:
- Dynamic views to identify associated instability
- MRI:
- 21% asymptomatic individuals aged 60 to 80 years have evidence of lumbar stenosis
- CT +/- myelogram alternative if MRI not available
Management
- Non-operative:
- Indication
- Mild-to-moderate symptoms of neurogenic claudication
- Activity modification & relative rest
- Activity as soon as tolerated
- Avoidance of aggravating activities such as heavy lifting & excessive trunk extension, that decrease AP diameter of spinal canal
- Weight loss
- Patient education
- Physiotherapy
- Flexion-based exercises
- Stretching of hip flexors, hamstrings & paraspinal muscles, & strengthening of abdominal & trunk muscles
- Postural correction
- Hydrotherapy
- Elastic lumbar binder may provide benefit by reducing loads across lumbar spine, but it should be worn only for a short period of time in order to avoid deconditioning of paraspinal muscles
- Paracetamol & NSAIDs
- Muscle relaxants
- Tricyclic antidepressants
- Narcotic medications
- Sparingly & for only brief periods for patients with incapacitating pain who cannot tolerate NSAIDs
- Epidural steroid injections
- Decrease spinal stiffness & can facilitate eventual progression to active phase of therapy
- Although interlaminar & caudal routes of epidural injection are technically easier than injection through arthritic posterior elements in elderly patients with spinal stenosis, acute radicular pain in a specific nerve-root distribution is best treated with a transforaminal selective nerve-root injection (corticosteroid & bupivacaine) performed under fluoroscopic guidance
- A selective nerve root block is a good prognosticator of surgical outcome, as patients who obtain >50% relief of leg pain for at least 1 week tend to have ≥50% relief of leg pain, compared with preoperative intensity, within 1 month after surgery & lasting at least 6 months postoperatively
- Prognosis
- 70% substantial decrease in symptoms & avoidance of surgery
- Indication
- Operative:
- Indications
- Patients who are functionally limited in terms of both walking tolerance & ADLs
- Intractable pain, especially neurogenic claudication (leg or buttock pain), that has not responded to non-operative treatment
- Urgent surgical decompression with a rapidly progressive neurologic deficit &/or cauda equina syndrome (bladder & bowel dysfunction); however this is rare
- Perfect surgical candidate
- Severe leg symptoms of a neurogenic claudicatory nature & corresponding stenosis on imaging studies
- No or minimal axial back pain
- No or minimal neurologic deficit
- No evidence of vascular claudication
- No medical comorbidities
- Principles
- Even when symptoms are unilateral, bilateral decompression should be performed if there is radiographic evidence of bilateral stenosis because contralateral symptoms will soon develop
- Another important goal of surgical treatment of stenosis is maintenance of stability of spinal column, which can be facilitated during the decompression by clear identification & preservation of pars interarticularis & by undercutting & preserving at least lateral 50% of facet joints
- Fusion +/- instrumentation recommended to maintain stability with complex stenosis associated with degenerative spondylolisthesis or degenerative scoliosis (a curve of >30°) or if >50% of facet joints are removed bilaterally during decompression
- Indications
- Technique (laminectomy)
- Loupe magnification
- Prone kneeling position on an Andrews frame to minimise intra-operative bleeding from epidural venous plexus; if internal fixation is planned, a more lordotic position on a Jackson table may be preferred, but more blood loss can be expected
- Midline incision
- Dissection to lumbodorsal fascia
- Subperiosteal dissection exposing spinous processes & lamina
- Lateral radiograph to identify correct level (attach towel clip)
- Dissection is then carried out laterally superficial to facet joints, with care taken to preserve facet joint capsules & to identify pars interarticularis
- Parafacetal arteries that lie medial & lateral to facet joints may cause additional hemorrhage during lateral dissection, but bleeding can be easily controlled with electrocautery
- If a posterolateral fusion is planned, lateral dissection needs to extend to the tips of the transverse processes bilaterally, while intertransverse membrane is maintained
- Inferior half of spinous process at top of decompression & superior half of spinous process of inferior level to be decompressed are removed
- Intervening spinous processes excised
- Any remaining soft tissue removed & lamina thinned
- Bone wax applied to bleeding bone allows maintenance of a dry surgical field
- Ligamentum flavum is identified, & a dissector or curette is used to gently dissect insertion of ligament from undersurface of inferior edge of most caudal lamina, where a central decompression begins
- Removal of laminae should always start centrally, since midline is last area to become stenotic & thus safest place to begin dissection
- Dura protected as decompression extended laterally to pedicles
- Medial facetectomy & removal of any osteophytic ridge adjacent to intervertebral disc space
- Midzone, located anterior to pars interarticularis & inferior to pedicle, can be decompressed with undercutting of hypertrophic facet joints & area under pars interarticularis with a small Kerrison rongeur
- Nerve roots are identified, & neural foramen is probed to make sure it is adequately patent
- Probe should be passed in an inferolateral direction parallel to course of nerve root
- Discectomy
- Performed only if necessary to further decompress both exiting & traversing nerve roots & only for extruded soft disc material or a free fragment, since violation of degenerated, well-contained discs may lead to unnecessary destabilisation of anterior column
- Bilateral laminotomies alternative
- Potential for postoperative iatrogenic spondylolisthesis is reduced by performance of laminotomies, which preserve midline stabilising structures
- Indications for fusion
- Instability at involved motion segment
- Degenerative scoliosis (especially with curve progression or a curve magnitude of >30°)
- Revision decompression at same level, resection of >50% of facets bilaterally
- ® Degenerative spondylolisthesis
- Prognosis
- Relief of back pain in 80%
- Relief of leg symptoms in 95%
- Good or excellent outcome in 85% after 4 years
- Best results obtained when surgical intervention carried out within 1st few years after onset of disease
- Prolonged structural compromise of spinal nerve roots may lead to chronic & irreversible damage that surgical decompression cannot correct
- ® Results of surgical decompression are usually better if procedure is performed within a year after onset of symptoms
- Post-operative care
- Mobilise day 1 post-operatively
- Avoid bending, lifting or twisting for 6 to 12 weeks
- Radiographs to monitor for instability or hardware failure
- Complications
- Epidural hematoma
- Thromboembolic event
- Dural tear (especially in revisions)
- Infection
- Instability following wide decompression
- Nerve root injury
- Nonunion or hardware failure following fusion
- Adjacent segment degeneration
- Recurrence of symptoms
- Prognosis
Summary
IMAGE MISSING
