Diagnosis and Treatment
Cervical radiculopathy, commonly called a "pinched nerve", occurs when a nerve in the neck is compressed or irritated where it branches from the spinal cord. This may cause pain that radiates into the shoulder, as well as muscle weakness and numbness that travels down the arm and into the hand or fingers. It is often caused by "wear and tear" changes that occur in the spine as we age, such as arthritis. In younger people, it is most often caused by a sudden injury that results in a herniated disc.
Most cases of cervical radiculopathy respond well to conservative treatment that includes medication and physical therapy.
Anatomy
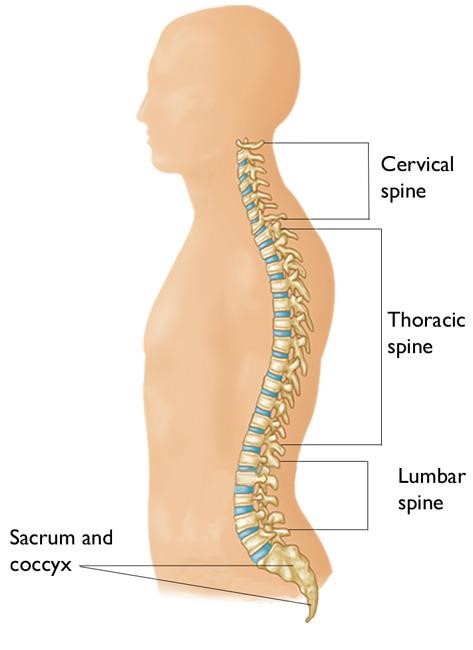
Your spine is made up of 24 bones, called vertebrae, that are stacked on top of each other. These bones connect to create a central canal that protects the spinal cord. The seven small vertebrae that begin at the base of the skull and form the neck comprise the cervical spine.
orthoinfo.aaos.org
Other parts of your spine include:
- Spinal cord and nerves - These "electrical cables" travel through the spinal canal carrying messages between your brain and muscles. Nerve roots branch out from the spinal cord through openings in the vertebrae (foramen).
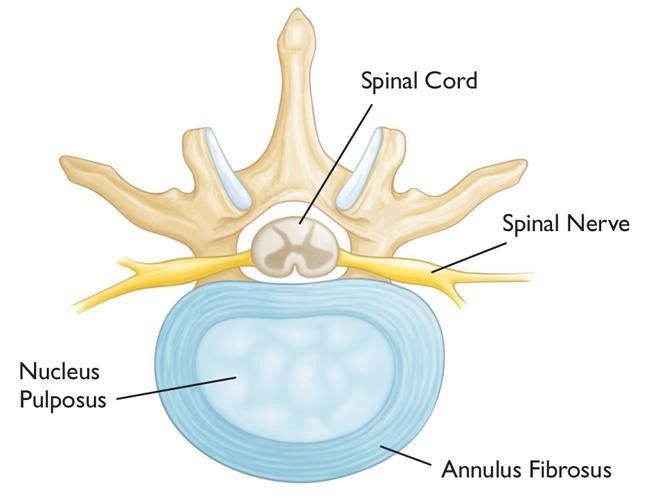
- Intervertebral discs - In between your vertebrae are flexible intervertebral discs, which act as shock absorbers. Intervertebral discs are flat and round and about 5-10mm thick. They are made up of two components:
- Annulus fibrosus - the tough, flexible outer ring of the disc.
- Nucleus pulposus - the soft, jelly-like centre of the disc.
orthoinfo.aaos.org
A healthy intervertebral disc (cross-section view).
Cause
Cervical radiculopathy most often arises from degenerative changes that occur in the spine as we age, or from an injury that causes a herniated, or bulging, intervertebral disc.
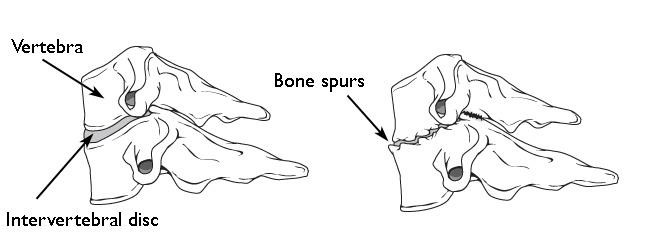
Degenerative changes
As the discs in the spine age, they lose height and begin to bulge. They also lose water content, begin to dry out, and become stiffer. This problem causes settling, or collapse, of the disc spaces and a loss of disc space height, which results in the vertebrae moving closer together. The body responds to the collapsed disc by forming more bone (called bone spurs) around the disc to strengthen and stabilise the area. These bone spurs may also narrow the foramen (the small openings on each side of the spinal column where the nerve roots exit) and pinch the nerve root. Degenerative changes in the disks are often called arthritis or spondylosis. These changes are normal and they occur in everyone. In fact, nearly 50% of all people middle-aged and older have worn discs and pinched nerves that do not cause painful symptoms. It is unclear as to why some patients develop symptoms and others do not.
 orthoinfo.aaos.org
orthoinfo.aaos.org
(Left) Side view of a healthy cervical vertebra and disc. (Right) A disc that has degenerated and collapsed.
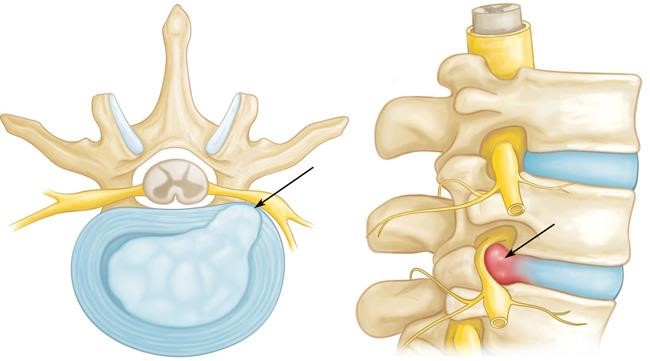
Herniated disc
A disk herniates when its jelly-like centre (nucleus pulposus) pushes against its outer ring (annulus). If the disc is very worn or injured, the nucleus may squeeze all the way through. When the herniated disk bulges out toward the spinal canal, it puts pressure on the sensitive nerve root or spinal cord, causing pain and weakness in the area the nerve supplies. A herniated disk often occurs with lifting, pulling, bending, or twisting movements.
orthoinfo.aaos.org
In a herniated disk, the soft, jelly-like centre of the disc can push all the way through the outer ring. (Cross-section and side views shown)
Symptoms
In most cases, the pain of cervical radiculopathy starts at the neck and travels down the arm in the area served by the damaged nerve, and is usually described as burning or sharp. Certain neck movements, such as extending or straining the neck or turning the head, may increase the pain. Some patients report a decrease in pain when they place their hands on top of their head, a movement that may temporarily relieve pressure on the nerve root.
Other symptoms include:
- Tingling or the feeling of "pins and needles" in the fingers or hand
- Weakness in the muscles of the arm, shoulder, or hand
- Loss of sensation
Diagnosis and Investigation
As with most orthopaedic conditions, a full and thorough history and examination is most important in making the diagnosis of cervical radiculopathy. Following this, a number of specific tests and imaging studies may be needed, and can include:
-
X-rays - These provide images of dense structures, such as bone. An x-ray will show the alignment of bones along your neck, and can demonstrate functional instability. It can also reveal whether there is any narrowing of the foramen and damage to the discs.
-
Computed tomography (CT) scans
-
Magnetic resonance imaging (MRI) scans - An MRI of the neck can show if your nerve compression is caused by damage to soft tissues, such as a bulging or herniated disc, and can also help determine whether there is any damage to your spinal cord or nerve roots.
-
Nerve conduction study and/or Electromyography (EMG).
Treatment
The majority of patients with cervical radiculopathy get better over time and do not need treatment. It is also common for cervical radiculopathy that has improved to return at some point in the future. Even when this occurs, it usually gets better without any specific treatment.
Nonsurgical Treatment
Initial treatment for cervical radiculopathy is nonsurgical. Nonsurgical treatment options include:
- Soft cervical collar - This is a padded ring that wraps around the neck and is held in place with Velcro. The collar allows the muscles in your neck to rest and to limit neck motion, which can help decrease the pinching of the nerve roots that accompany movement of the neck. A soft collar should only be worn for a short period of time since long-term wear may decrease the strength of the muscles in your neck.
- Physical therapy - Specific exercises can help relieve pain, strengthen neck muscles, and improve range of motion. Occasionally, traction can be used to gently stretch the joints and muscles of the neck.
- Medications – These may include:
- Simple analgesia, such as Paracetamol
- Nonsteroidal anti-inflammatory drugs (NSAIDs) – NSAIDs may provide relief if your pain is caused by nerve irritation or inflammation.
- Oral corticosteroids - These may help relieve pain by reducing swelling and inflammation around the nerve.
- Steroid injection - In this procedure, steroids are injected in the foramen near the affected nerve or into the adjacent facet (zygapophyseal) joint to reduce local inflammation. Although steroid injections do not relieve the pressure on the nerve caused by a narrow foramen or by a bulging or herniated dis, they may lessen the swelling and relieve the pain long enough to allow the nerve to recover.
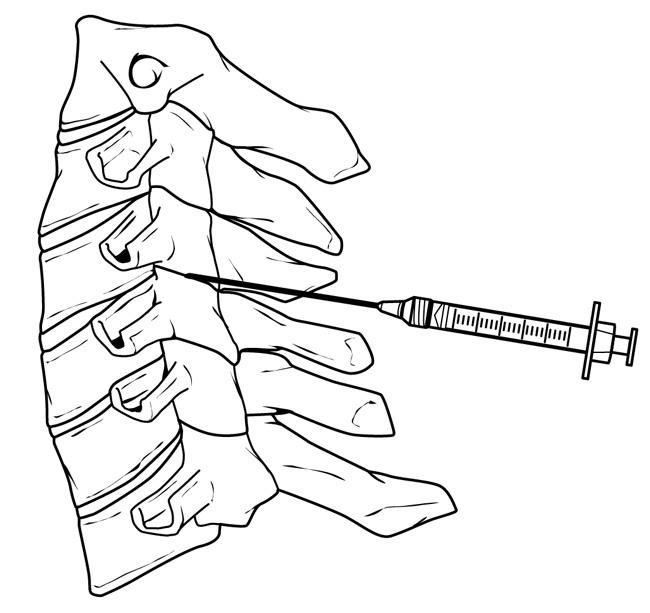 orthoinfo.aaos.org
orthoinfo.aaos.org
Facet joint injection in the cervical spine.
-
- Narcotics - These medications are reserved for patients with severe pain not relieved by other options, and are usually prescribed for a limited time only.
Surgical Treatment
If nonsurgical treatment does not relieve symptoms after a period of time, surgery may be recommended. There are several surgical procedures to treat cervical radiculopathy, and the option chosen will depend on many factors, including what symptoms you are experiencing and the location/level of the involved nerve root.
The primary goal of surgery is to relieve symptoms by decompressing, or relieving pressure on, the compressed nerves in your neck. Other goals of surgery include:
- Improving neck and referred arm pain
- Maintaining stability of the spine
- Improving alignment of the spine
- Preserving range of motion in the neck
In most cases, surgery for cervical radiculopathy involves removing pieces of bone or soft tissue (such as a herniated disc), or both. This relieves pressure by creating more space for the nerves to exit the spinal canal.
Surgical Procedures
There are three main surgical procedures commonly performed to treat cervical radiculopathy. They are:
- Posterior Cervical Laminoforaminotomy (or Laminectomy)
- Anterior Cervical Discectomy and Fusion (ACDF)
- Artificial Disc Replacement (ADR)
1. Posterior Cervical Laminoforaminotomy
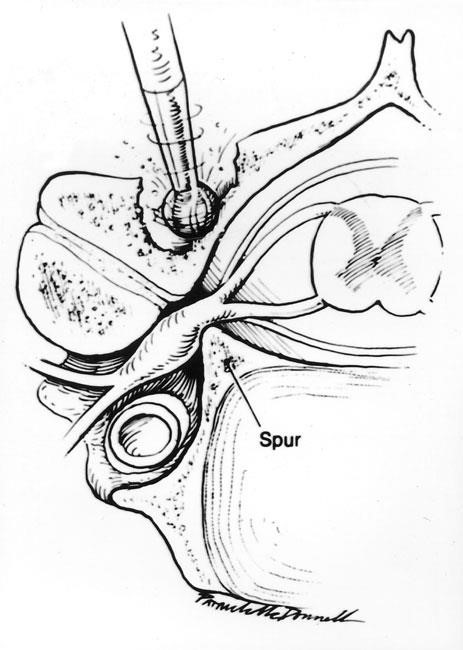
orthoinfo.aaos.org
In posterior cervical laminectomy or laminoforaminotomy, special tools are used to thin down the lamina to gain better access to the nerve.
2. Anterior Cervical Discectomy and Fusion (ACDF)
ACDF is the most commonly performed procedure to treat cervical radiculopathy. The procedure involves removing the problematic disc or bone spurs via an anterior (front of neck) approach and then stabilizing the spine through spinal fusion.
The goals of ACDF are to restore alignment of the spine, maintain or enlarge the space available for the nerve roots to leave the spine, and limit motion across the degenerated segment of the spine.
The "anterior" approach is performed through a 4-5cm incision along the neck crease, most safely done on the left side of the neck. The relevant level is confirmed with intra-operative X-ray control. The problematic disc and any additional bone spurs are removed, the disc space is restored to the height it was prior to the disc wearing out, and this creates more room for the nerves to leave the spine and aids in decompression. A spinal fusion is used to stabilize the spine, with the basic concept being to fuse together the vertebrae so that they heal into a single, solid bone. Fusion eliminates motion between the degenerated vertebrae and takes away some spinal flexibility. The theory is that if the painful spine segments do not move, they should not hurt. A metal or plastic spacer (or cage) filled with bone graft (or combined with synthetic bone graft substitute) is impacted into the defect prepared after removal of the old disc, and supplemental fixation in the form of a plate and screws is also added.

orthoinfo.aaos.org
An anterior cervical discectomy and fusion from the side (left) and front (right). Plates and screws are used to provide stability and increase the rate of fusion.
3. Artificial Disk Replacement (ADR)
This procedure involves removing the degenerated disc and replacing it with artificial parts, as is done in hip or knee replacement. The goal of disc replacement is to allow the spinal segment to keep some flexibility and maintain more normal motion, which may relieve some pressure on the adjacent disc levels and prevent them from premature failure.
Similar to ACDF, an "anterior" approach is used for the surgery. The problematic disc level is removed after confirmation with intra-operative X-ray, and then an artificial disc implant is inserted into the disc space. The implant is made of all metal, metal and plastic, or metal and ceramic. It is designed to maintain motion between the vertebrae after the degenerated disc has been removed. The implant may help restore the height between the vertebrae and widen the passage for the nerve roots to exit the spinal canal.
 orthoinfo.aaos.org
orthoinfo.aaos.org
Side and front view of patient with artificial disc replacement.
Risks and Complications
As with any surgical procedure, there are risks associated with cervical spine surgery. Possible complications can be related to the approach used, the bone graft, healing, and long-term changes. A/Prof Woodgate will discuss the risks with you prior to surgery, and will take specific measures to help avoid potential complications.
General Risks
The possible risks and complications for any cervical spine surgery include:
- Infection
- Bleeding
- Nerve injury
- Spinal cord injury
- Reaction to anaesthesia
- The need for additional surgery in the future
- Failure to relieve symptoms
- Tear of the sac covering the nerves (dural tear)
- Life-threatening medical problems, such as heart attack, lung complications, or stroke
Anterior Cervical Discectomy and Fusion and Artificial Disc Replacement Risks
There are additional potential risks and complications when an anterior approach is used in spine surgery. They include:
- Misplaced, broken, or loosened plates, screws, or implants
- Soreness or difficulty with swallowing
- Voice changes
- Breathing difficulty
- Injury to the oesophagus
- Pain at the donor site of any bone graft (if an autograft is used)
- Non-union of the spinal fusion (in ACDF)
- Loosening of the artificial disc replacement
Recovery
After surgery, you will typically stay in the hospital for 2 or 3 days. Most patients are able to walk and eat on the first day after surgery. It is normal to have difficulty swallowing solid foods for a few weeks or have some mild hoarseness following anterior cervical spine surgery. You will need to wear a soft cervical collar for 6 weeks. After spinal fusion, it may take from 6 to 12 months for the bone graft to become solid, and you will have specific restrictions for some time period after your surgery. Most people are able to return to a desk job within a few weeks after surgery. They may be able to return to full activities by 3 to 4 months, depending on the procedure. For some people, healing may take longer.
